Why Exercise Fails for Some: The Gut–Adipose–Inflammation Axis in Insulin Resistance
- Jigar Thakkar
- Dec 23, 2025
- 3 min read
Introduction
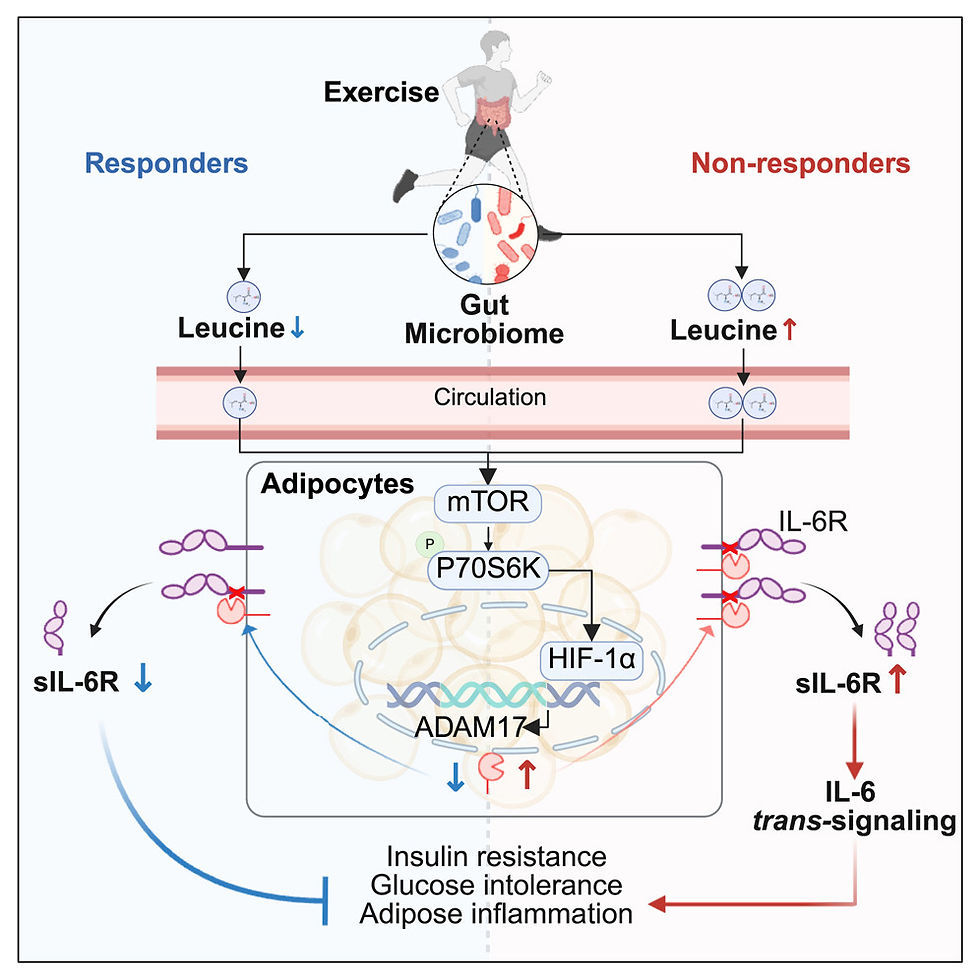
Exercise is widely prescribed to improve insulin sensitivity and glycemic control, especially in individuals with obesity and metabolic disorders. However, clinical observations show that not everyone responds metabolically to exercise in the same way. Recent research highlights a novel mechanism explaining this variability — a crosstalk between the gut microbiome and adipose tissue that modulates inflammation and insulin action.
This study uncovers how changes in the soluble interleukin-6 receptor (sIL-6R) determine whether exercise improves or worsens metabolic outcomes.

Key Concept: Exercise Responders vs Non-Responders
Individuals were categorized based on their metabolic response to structured exercise:
Responders (R): Improved insulin sensitivity and glycemic control
Non-Responders (NR): No improvement or worsening of glucose metabolism
The differentiating factor was not exercise adherence, but molecular and microbial differences
Role of Soluble IL-6 Receptor (sIL-6R)
sIL-6R is a circulating receptor that enables IL-6 trans-signaling, a pro-inflammatory pathway
Findings showed:
Responders experienced a reduction in sIL-6R levels after exercise
Non-responders showed a significant increase in sIL-6R
Elevated sIL-6R was directly associated with:
Increased inflammation
Reduced insulin sensitivity
Poor glycemic control despite exercise

Mechanism: Gut Microbiome–Adipose Communication
1. Gut Microbiome Produces Leucine
In non-responders, the gut microbiome produces higher levels of the amino acid leucine.
This leucine acts on white adipocytes (fat cells). Walter Sport
2. Activation of Intracellular Pathway
Leucine stimulates the mTOR-HIF1α signaling pathway inside adipose tissue cells.
This leads to activation of ADAM17, an enzyme that cleaves IL-6R off the cell surface, increasing circulating sIL-6R. LinkedIn
3. Impact on Inflammation & Insulin Sensitivity
Elevated sIL-6R increases IL-6 trans-signaling, which promotes adipose inflammation.
This inflammation interferes with exercise-induced improvements in glucose regulation and insulin sensitivity. PubMed
Impact on Insulin Sensitivity and Glycemic Control
Elevated IL-6 trans-signaling:
Promoted adipose tissue inflammation
Impaired insulin signaling pathways
Reduced glucose uptake in peripheral tissues
As a result, exercise failed to deliver its expected metabolic benefits in non-responders
Experimental Validation
Human studies showed consistent correlations between sIL-6R levels and metabolic outcomes
Animal models confirmed causality:
Fecal microbiota transplantation from non-responders transferred exercise resistance
Adipose-specific deletion of ADAM17 restored insulin sensitivity
Blocking IL-6 trans-signaling reversed exercise non-responsiveness
Why This Research Is Important
Explains why exercise alone is not universally effective
Identifies sIL-6R as a potential biomarker for exercise responsiveness
Highlights the gut microbiome as a modifiable therapeutic target
Supports the need for personalized metabolic interventions
Clinical and Functional Medicine Implications
Metabolic health strategies may need to include:
Gut microbiome modulation (diet, prebiotics, probiotics)
Anti-inflammatory nutritional approaches
Targeted support for adipose tissue signaling
Exercise prescriptions should be customized, not generic
Conclusion
This research reshapes how we view exercise in metabolic health. The effectiveness of physical activity is deeply influenced by gut–adipose tissue communication and inflammatory signaling pathways. Elevated soluble IL-6 receptor levels, driven by microbiome-derived metabolites, can blunt the metabolic benefits of exercise.
Understanding this gut–fat axis opens the door to precision nutrition, targeted lifestyle interventions, and personalized exercise strategies, ensuring that exercise truly works for improving insulin sensitivity and glycemic control — not just in theory, but in practice.
TO SUM IT UP:
Responders show ↓ sIL-6R
Non-responders show ↑ sIL-6R
Gut microbiota in non-responders produce more leucine, activating the mTOR–HIF1α–ADAM17 pathway in adipose tissue → increased sIL-6R release.
Elevated sIL-6R triggers inflammation and weakens insulin signaling, offsetting exercise benefits.
Blocking ADAM17 or sIL-6R in mice reverses these metabolic defects.






Comments